Option Card: Metoidioplasty with scrotoplasty and closure of the vagina and two testicular implants
Print or save Option Card:
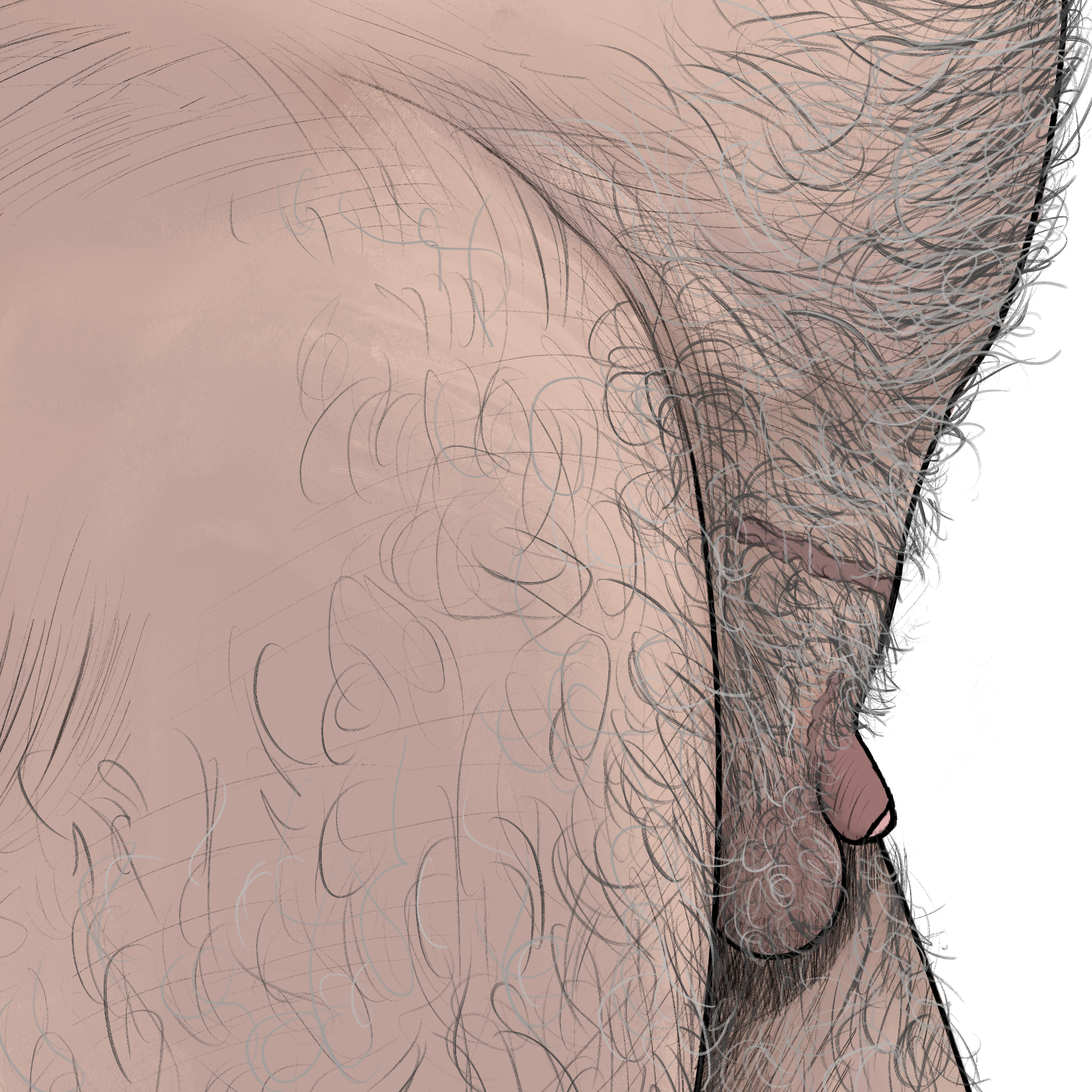
Metoidioplasty with scrotoplasty and closure of the vagina and two testicular implants
Metoidioplasty with scrotoplasty and vaginectomy and two testicular implants, but without urethral lengthening
What does the option involve?
- This surgery creates a penis which is not as large as most adult penises, creates a scrotum, closes your vaginal canal, and places two testicular implants.
- Your surgeon will release the erectile body (clitoris) by cutting the attachments that hold it in place. It can then be covered with genital skin.
- Your labia majora will be used to create the scrotum, and your labia minora will be used to cover the area where the labia majora used to be.
- The outer layer of tissue in the vagina will be removed, then the walls will be fused together.
- Two testicular implants will be placed into the scrotum after it has fully healed.
How many surgeries are needed?
- This process creates a penis in the first stage, and inserts testicular implants in the second stage.
Will I be able to stand to pee?
- Unless this was already possible with your anatomy, you will still need to sit to pee unless you use a stand-to-pee device.
Can I pee from the tip of my penis?
- No. Urethral lengthening is needed to pee though the tip of your penis.
- You may continue to pee from the same place that you currently pee from, but your urethra may be slightly moved or lengthened as a result of the vaginectomy; discuss this with your surgeon.
How long will my penis be?
- If your penis has enough length, and you do not have complications that prevent you from doing so, it may be possible for you to stand to pee.
- However, less than 20% of patients with a 2 to 4 centimeters (0.79 to 1.57 inches) pre-surgery penis size can stand to pee through their pants’ fly.*
- Seventy percent of patients with a pre-surgery erectile body size of about 2 centimeters (0.79 inches) and a prominent mons can stand to pee by lowering their pants, but they won’t necessarily be able to pee standing up with their penis through the zipper of their pants.*
Will I be able to feel temperature sensation, tactile sensation, and pain sensation in my penis? Can I have an orgasm, or feel erogenous sensation with my penis?
- Surgeons think that there’s a more than 90% chance that you’ll be able to feel touch in your penis after the surgery.*
Can I have an orgasm, and/or feel erogenous sensation with my penis?
- Surgeons think that there’s a more than 90% chance that you’ll be able to feel erogenous sensation in your penis after the surgery.*
- If you were able to orgasm before surgery, you will likely still be able to do so after surgery.
Will I be able to have an erection?
- Surgeons think that there’s a more than 90% chance that your penis will be able to get ‘hard’ (have an unassisted erection) without an internal implant or external prosthetic after surgery.*
Will I be able to penetrate a partner during sex?
- Depending on your size before surgery, and the body type of you and your partner, you may be able to put your penis inside your sex partner in some positions.
- However, there’s less than a 5% chance that you’ll be able to vaginally or anally penetrate a partner with your penis while erect (without using an external device) after surgery.*
- However, surgeons think that there’s less than a 5% chance that you’ll be able penetrate a partner with your penis while erect (without using an external device) after surgery.*
- You can also penetrate your partner during sex with your fingers or a prosthetic that is meant to be used during sex.
- Some prosthetics may be worn over the penis and act as a penis extension, but they do not stay attached well enough to easily vaginally or anally penetrate a partner.
Will I be able to have testicular implants?
- Yes. You will be able to have two testicular implants placed in your scrotum at least 6 months after the scrotum was created.
Will I be able to become pregnant and carry and birth a child via the vaginal canal?
- No. Closure of the vagina means you will not be able to be vaginally penetrated.
Will I be able to become pregnant and carry and birth a child via the vaginal canal?
- No. Closure of the vagina means you will not be able to carry a child. Talk about your fertility goals with your doctor.
What will I need to do before surgery?
- Many surgeons and insurance companies will require that you provide one or more letters from mental health providers as per The World Professional Association for Transgender Health (WPATH)’s Standards of Care (SOC).
Is there a BMI (body mass index) requirement for this surgery?
- Many surgeons have a specific BMI requirement of 35 or below, although it can vary.
- Surgeons will also evaluate patient’s health on a case-by-case basis and may require that any comorbidities correlated with a higher BMI are well-managed to reduce the risk of complications from surgery.
Do I need a hysterectomy or oophorectomy?
- You need a hysterectomy if you will be getting closure of the vagina. Your uterus and cervix will need to be removed, and you may also have your fallopian tubes removed.
- You can choose to keep your ovaries if you don’t want an oophorectomy.
Do I need to stop using nicotine before surgery?
- Yes, you will need to stop using nicotine for 8 to 12 weeks before surgery. This includes cigarettes, vapes, gum, patches, wraps and e-cigarettes. You should discuss other substance use with your surgeon before surgery.
Do I need to stop taking hormones before surgery?
- No, most people do not need to stop taking testosterone before surgery. You should discuss your medications with your surgeon to see if any need to be stopped before surgery.
Is hair removal is needed?
- Hair removal is not medically necessary, but some people choose to have hair removal done on their scrotum for aesthetic reasons. This is typically not covered by insurance.
How long is the hospital stay?
- You may stay 2-3 days in the hospital after your surgery.
Will I need to stay near the hospital?
- You may need to stay near the hospital for the first 2-4 weeks after surgery.
Will I need a caretaker when I get home?
- A caregiver can be helpful for the first week after surgery.
How long will it take to recover once I’m at home?
- You may be able to return to most of your daily activities, including work, after four to six weeks. Some people with very physically demanding jobs may need longer than six to eight weeks.
Is medical tattooing needed?
- Medical tattooing is not needed.
What will happen with my labia minora?
- Part of the tissue is used for the metoidioplasty and part is used to cover the area where the majora were moved. This is why it will appear as if the folds of your labia minora are gone. Your vulva will be stretched open and may become more dry.
What appointments will I have before surgery and after surgery?
- You will have at least two appointments before surgery, and several post-operative appointments after surgery.
Will I need a urethral catheter or a suprapubic catheter?
- You will have a urethral catheter in place for 5-7 days.
- You will not need a suprapubic catheter.
Learn more about catheters here:
Will I have a donor site?
- No, you will not have a donor site if you do not get phalloplasty.
What is the risk of urethral stricture or fistula preventing peeing from the tip of penis?
- You will not have a fistula or stricture if you do not have urethral lengthening. You may experience bladder spasms or an infection from the urethral catheter.
What is the risk of developing a wound complication?
- Up to 30% of patients might have a wound problem (like bleeding or infection) after metoidioplasty, not including problems with the urethra if urethral lengthening is performed.*
- Less than 5% of patients will have a wound problem (like bleeding or infection) that needs more surgery after metoidioplasty, not including problems with the urethra if urethral lengthening is performed.*